Regional Disaster Health Response System Demonstration Sites Provide Critical Support By Coordinating Information Sharing Efforts and Technical Assistance Throughout Pediatric Surge
Fall 2022 - Spring 2023
Impact
Regional Disaster Health Response System (RDHRS) demonstration sites provided critical support for hospitals and clinicians throughout the pediatric surge caused by RSV (respiratory syncytial virus) in 2022. The RDHRS sites worked to enhance situational awareness within their regions by standing up patient tracking dashboards, developing and disseminating pediatric surge tools and resources, and hosting meetings with all response partners to provide technical assistance and real-time updates on regional surge status. Leveraging their robust partner networks, the RDHRS sites increased bidirectional communication between all entities and organizations involved in pediatric surge response, supporting a well-informed and organized system that prioritized timely and effective patient care.
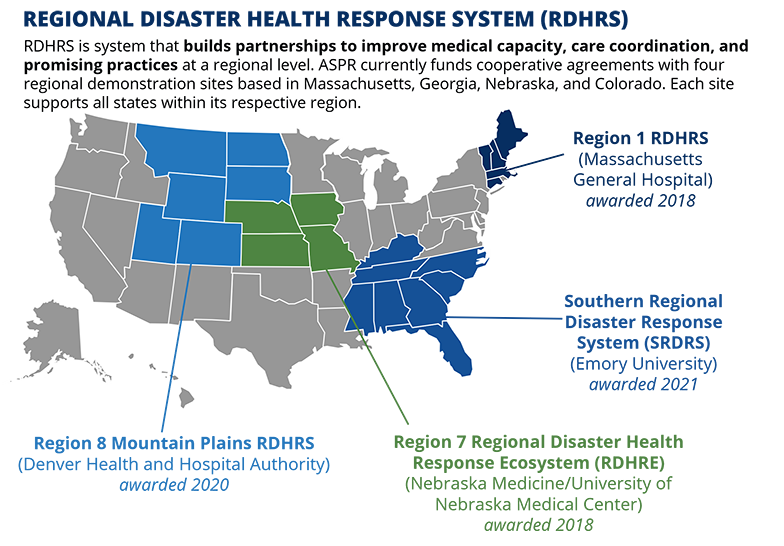
Since Fiscal Year 2018, ASPR has continued to establish RDHRS sites
across the country. For more information on RDHRS sites and
activities, head to the RDHRS Webpage
|
Background
As the 2022-23 school year began, the spread of respiratory viruses such as RSV and influenza accelerated, causing a sharp demand for pediatric acute care services across the country. ASPR’s RDHRS demonstration sites sprang into action, working together with the Pediatric Centers of Excellence as well as partners across health care and public health, to support the pediatric surge and help ensure timely and accessible care to patients in need.
Response:
Region 1 Regional Disaster Health Response System:
The
Region 1 RDHRS worked tirelessly to bolster situational awareness across Region 1 hospitals, developing resources and tools to assist hospitals, health care coalitions, public health departments, and other health professionals throughout the pediatric surge. During the surge, community hospital clinicians described needing to make many calls to find an inpatient bed for their pediatric patients. Region 1 RDHRS, in collaboration with ASPR Region 1, created a web-based pediatric patient transfer availability tool that helped community clinicians better identify which pediatric hospitals were able to take transfers at any point in time. Across the region, there were over 200 people registered for the tool. Region 1 RDHRS also built pediatric-specific adaptations to its disaster telehealth tool which could enable regional pediatric referral centers to provide intensivist guidance to clinicians across the region. Finally, the Region 1 RDHRS worked with Regional Emergency Medical Services for Children (EMSC) leads across New England to put together a
six-part educational webinar series which focused on building additional clinical and operational capabilities to manage pediatric patients with acute respiratory illness. The series had over 1,800 participants and brought timely guidance to intensivists on the front lines. In addition to all of their efforts, the Region 1 RDHRS continuously updated its website with links to pediatric surge resources and the Pediatric Centers of Excellence, providing timely and relevant information to support the response.
Region 7 Regional Disaster Health Response Ecosystem:
The Region 7 Regional Disaster Health Response Ecosystem (RDHRE) leveraged its assets to enhance situational awareness throughout the pediatric surge. Region 7 RDHRE hosted the Region 7 Pediatric Acute Care stakeholders on routine calls which convened practitioners from all major children’s hospitals and any acute care hospitals with pediatric beds, public health partners, health care coalition coordinators, regional ASPR representatives, and hospital associations in the region. During these calls, pediatric experts shared promising practices on topics such as: informing adult critical care practitioners on relevant pediatric care; troubleshooting supply and equipment shortages; identifying barriers with patient movement; and brainstorming safe staffing models for hospitals. In addition to these calls, the Region 7 RDHRE collaborated with all 22 pediatric hospitals and six pediatric transport teams in the region to develop situational reports detailing hospital capacity as well as challenges with staffing, bed availability, and supply shortages. The team also identified additional transport services and resources, ensuring hospitals in the region had backup options, should state-based transport teams be unavailable to help. Finally, the Region 7 RDHRE stood up a rapid pediatric bed availability dashboard for the region, a resource that helped hospitals identify where to transfer patients, during times of surge.
Region 8 Mountain Plains Regional Disaster Health Response System:
The Region 8 Mountain Plains RDHRS supported hospitals across the region by aligning hospital surge data, identifying and sharing pediatric specific trainings and resources, and providing technical support. The Region 8 RDHRS supported data collection on the RSV surge and pediatric bed availability across the region and surrounding states and worked with two major children’s hospital transfer centers which identified available beds in the region. To supplement the situation reports, and at the request of partners, the Region 8 RDHRS facilitated a weekly meeting between Primary Children's Hospital, Children's Hospital – Colorado, the Colorado Department of Public Health & Environment (CDPHE), and the Utah Department of Health and Human Services to discuss situational awareness, ongoing challenges, load balancing, and best practices. The team also provided technical support to the CDPHE Medical Operations Center by developing recommendations for use of adult intensive care unit (ICU) beds for pediatric patients, pediatric staffing considerations, and pediatric respiratory patient training modules by activating the Medical Advisory Panel (MAP). In addition, the Region 8 RDHRS coordinated and planned for the Region 8 Pediatric Town Hall with partners from the Pediatric Pandemic Network and ASPR Region 8.
Region 4 Southern Regional Disaster Health Response System:
The Southern Regional Disaster Response System (SRDRS) supported the development and dissemination of several pediatric surge specific resources for practitioners and hospitals to reference. The SRDRS collaborated with the Regional Emerging Special Pathogen Treatment Center (RESPTC) based at Emory University to hold both a podcast and webinar highlighting promising practices on pediatric acute care basics for adult care specialists, resources on the clinical management of RSV, and hospital bed placement and patient transportation resources. In addition to these webinars, SRDRS shared recently published contingency planning resources surrounding the use of adult ICU beds for pediatric patients. Finally, the SRDRS worked to provide pediatric technical assistance to community partners, particularly for sites with less pediatric experience and exposure.
Read more about RDHRS pediatric surge response through the
recent post on ASPR's Blog.

